This Web-OFP site offers monthly cases that will be sent by e-mail for readers to review and study.
This 43 year old woman was seen for a complaint of continuous pain in the left mandible and numbness in the chin subsequent to dental implants. Tooth #21 was continuously painful, had been endodontically treated, and was recently evaluated with cracked tooth survey which did not reveal a crack. She had been treated in a pain clinic for 1 year prior to her referral to UCLA for a second opinion.
Medical History
Her past medical history for pain includes having RCT in a tooth in the lower left when she was a teenager and having ongoing pain afterwards. She has had dental implants done in the lower left to replace the teeth that had endodontic treatment and subsequently extracted. She indicated that her ongoing pain is exacerbated by bruxing, pushing on the left masseter muscle, cold, biting. It is decreased by applying cold to the area until it is numb. She also gets some relief by taking Vicodin which is used for cervical pain. Past treatments for the pain in the lower left area include capsaicin, Elavil to 80 mg/d, Neurontin up to 3200 mg/d, Tenormin 50 mg/d, Nardil, a stent with Orabase and Capsaicin, and methergine. At the evaluation visit, she was taking Synthroid, Claritin, Trilevelin, Vicodin, Soma, Lasix and Prilosec. Her past medical history includes arthroscopy of the left knee and she was hospitalized in February, 1995 for pneumonia and September 1995 for a broken ankle which was fractured when she fell while taking Nardil. She does not have children. She does not work due to depression and chronic back problems. At the evaluation visit, she was not taking any psychotropic medications. She reported no EENT problems. She reported that her jaw pops but she had no history of locking or pain in the jaw. She reported pain in her neck and back. She reported having hyperactive airway. She has a history of ulcers, but denied GU, Kidney or liver problems.
Examination
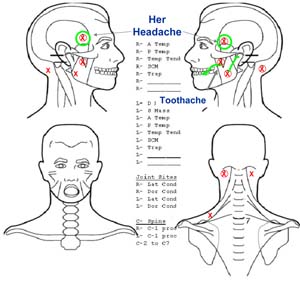
Cranial nerve screening examination was grossly intact except for decreased sensory response in left mental nerve distribution. Intraoral sensory testing was normal. No neurosensory symptoms were noted, i.e., no dysesthesia, static or dynamic allodynia, no pinprick hyperalgesia. Tooth number 21, the tooth in question, was tender to percussion but this did not replicate the chief complain.
The stomatognathic examination noted an unrestricted range of opening to 55 mm with no pain. Excursive movements were normal in extent and also without pain. No noises were noted in the TM joints. No joint sensitivity was noted with manipulation or palpation. Tongue/cheek ridging was moderate and dental attrition was severe.
Palpation of the masticatory muscle noted multiple MFP triggerpoints with radiation. Somatosensory blocking did not relieve the pain.

Radiographs
Implants placed in lower left mandible. These implants have not been restored due to the ongoing pain. Tooth number 21 has been treated endodontically for persistent pain and restored but the pain has not resolved.